The postpartum period is a transformative phase for new mothers, marked by a plethora of physiological and emotional changes as the body reverts to its pre-pregnancy state. One of the most pressing inquiries among new mothers is, “When does menstruation resume after childbirth?” This subject is often shrouded in ambiguity and can vary significantly from one individual to another. This guide seeks to elucidate the factors influencing the resumption of menstruation and the symbiotic relationship between hormonal changes and reproductive health following childbirth.
Typically, the menstrual cycle recommences in the months following the delivery of the baby, but myriad factors exist that can expedite or delay this process. Understanding these determinants is crucial for new mothers as they navigate their postpartum journey.
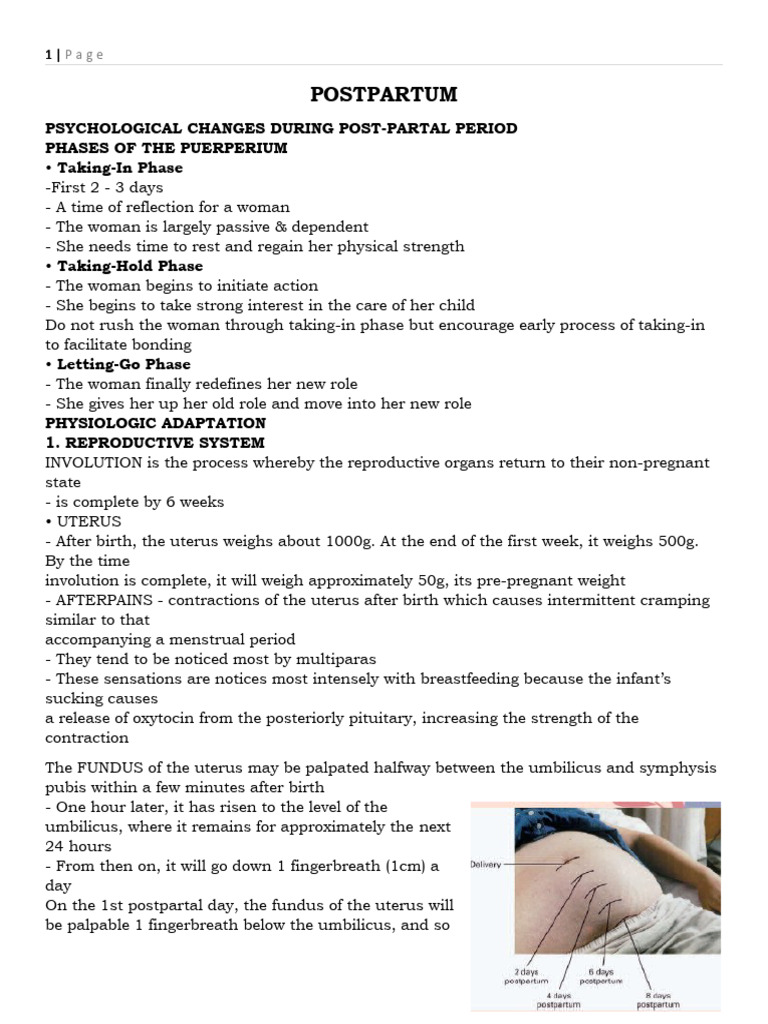
One of the primary factors affecting the timeline for the resumption of menstruation is whether the mother opts to breastfeed. Prolactin, a hormone released during breastfeeding, drastically inhibits ovulation, leading to a postponement of the menstrual cycle. Exclusive breastfeeding, especially in the initial months, can lead to the absence of menstruation for an extended period, often lasting from six months to over a year. This natural contraceptive mechanism is known as lactational amenorrhea. Unfortunately, the variance in how different bodies respond to lactation makes it impossible to predict the precise duration for each individual.
Moreover, it is essential to consider the frequency and duration of breastfeeding sessions. The more often an infant is breastfed, especially during the night, the higher the levels of prolactin and the longer the delay in the return of menstruation. Conversely, as breastfeeding becomes less frequent or as the infant begins to consume solid foods, prolactin levels decrease, which may trigger the return of menstrual cycles.
In contrast, mothers who choose to formula-feed their infants may experience the reintroduction of menstruation sooner, often within six to twelve weeks post-delivery. The absence of breastfeeding and its associated hormonal profiles allows the ovarian function to resume more rapidly.
Aside from breastfeeding practices, other physiological elements also influence the timeline of menstruation resumption after childbirth. For example, individual hormonal balances, age, pre-existing health conditions, and the specifics of previous menstrual cycles before pregnancy all contribute to variations in postpartum menstruation. Women with irregular cycles prior to pregnancy might observe fluctuations in timing once they have given birth.
The role of age cannot be overstated. As maternal age increases, the body’s hormonal balance may shift more dramatically, influencing the timing of menstrual return. Additionally, older mothers may experience more distinct perimenopausal symptoms, which can further obscure the onset of regular menstruation after childbirth.
Postpartum recovery encompasses more than just the physical. The emotional landscape can have profound implications on menstrual health. Stress—whether from the joys of welcoming a new life or the accompanying pressures—can lead to irregularities, including delayed menstruation. The body’s transition into motherhood, coupled with sleep deprivation and lifestyle changes, can profoundly impact hormonal rhythms, further complicating the timeline.
Another significant factor is the method of delivery. Research has shown that women who undergo cesarean sections may experience different hormonal shifts compared to those who have vaginal births. The surgical birth process can cause alterations in the normal healing mechanisms and hormonal release, potentially delaying the onset of menstruation.
As menstruation eventually resumes, new mothers might encounter changes in their menstrual cycle. It is not uncommon for cycles to be heavier, lighter, or more irregular than they were prior to pregnancy. The hormonal fluctuations resulting from breastfeeding and the body adjusting back to a non-pregnant state can contribute to these variations. Understanding that this is a normal part of the postpartum experience is essential for maintaining psychological well-being.
In some cases, underlying conditions such as polycystic ovary syndrome (PCOS) or thyroid irregularities may become more pronounced post-birth, potentially affecting menstrual cycles. Women with such conditions should maintain open lines of communication with their healthcare providers to monitor and manage their reproductive health as they transition through the postpartum phase.
It is imperative for new mothers to be cognizant of their bodies and their individual journeys through postpartum recovery. Tracking menstrual cycles can be valuable not just for family planning, but also for identifying any concerns regarding reproductive health. Utilizing tools such as fertility apps may help in understanding personal patterns and cycles.
In conclusion, the question of when menstruation resumes after childbirth does not have a unilateral answer. The interplay of breastfeeding, hormonal changes, maternal age, emotional well-being, and delivery methods all contribute to the diverse experiences encountered by new mothers. Each journey is unique, shaped by personal circumstances and choices. Ultimately, understanding these complexities can help alleviate anxiety and empower women during this monumental life transition.